Hoof Care
What is laminitis, or founder in horses and why is it so dangerous?
Edward Busuttil DVM CertAVP(EM) MRCVS, explains why laminitis should always be treated as an emergency
Laminitis also known as founder, – is one of every horse owner’s worst nightmares. Most of us have seen it and been frustrated by it but, how much do we really know about what is actually going on within the hoof?
Looking at the anatomy of what happens within the hoof will help develop an understanding of why this disease is so dangerous and, why it often carries a poor prognosis for returning to the same level of work and, a decreased quality of life.
In a quick comparison with our anatomy, while we generally have 5 fingers on each hand and 5 toes on each foot, horses stand on the equivalent to the tip of our middle finger or toe. The bone closest to the ground commonly has 4 names:
- Pedal bone
- Coffin bone
- Distal phalanx
- Third phalanx
All the names refer to the same bone. While we have nails on the dorsal aspect of our fingers and toes, the horse’s coffin bone is surrounded by a hoof.
The hoof functions to protect the coffin bone, cushion landing and, to ease breakover (the moment at which the last tip of a horse’s toe lifts off the ground). The horse’s weight is distributed between the digital cushion, sole and frog, with approximately 60% of a horse’s weight distributed between the front legs and, the rest between the hind legs. This helps to explain why laminitis mainly affects the front feet.
So how are the hoof wall and coffin bone connected?
Two layers of laminae (thin pleats) separate and hold together the hoof wall and coffin bone:
- The innermost layer, closer to the coffin bone, is called the sensitive, dermal layer, and it consists of blood vessels coming from the coffin bone. It develops from the coronet band.
- The outer layer is called the insensitive, epidermal layer. It is the innermost portion of the hoof wall. It receives nutrients from the sensitive layer.
The two sections are brought together by interdigitations of the layers (think interconnected fingers), held closely by special connective tissue and proteins called hemidesmosomes. Failure of this connection is what leads to the process of laminitis. As the name implies, laminitis is the inflammation of the laminae in the hoof. Inflammation presents as heat, pain, reddening, swelling and decreased function associated with a particular harmful agent.
What causes laminitis?
- Laminitis is caused by a number or combination of different pathways:
- Carbohydrate overload
- Uncontrolled endocrine disease (particularly Cushing’s and Equine Metabolic Syndrome).
- Obesity in horses and ponies (Excess weight) bearing due to a lesion in the opposing leg (an example is a fractured bone in the left fore might result in laminitis in the right fore)
- Serious systemic inflammation, particularly due to sepsis following infection such as pneumonia, colitis or metritis
“The SPEED at which treatment is initiated is ESSENTIAL in determining how a laminitic episode progresses”
An increase in age and increasing hours of sunshine (resulting in more sugars being present in the grass) also appear to be a risk factor for laminitis¹. There is only weak evidence supporting treatment with steroid therapy (either to treat systemic disease or as joint medication) as a causative of laminitis².
What actually happens?³
The development stage, which starts when the horse has a sugar overload or disease lasts 24-60 hours. During this time changes within cells at the border between the inner and outer layer of laminae start to develop. During this developmental stage, prevention of breakdown is possible, potentially through:
- Removing or treating the initiating cause of laminitis, including testing for metabolic disorders and, soaking hay for at least 8 hours to reduce sugars.
- Cryotherapy – cooling your horse’s legs downwards from the knee or hock by applying ice boots or having them stand in ice cold water for periods of time throughout the day.
- Providing deep bedding for your horse to stand on and encouraging them to lie down.
If the development stage is not contained, clinical signs associated with laminitis become apparent:
- Lameness
- Bounding digital pulses
- Possible response to hoof testers (but not always)
Again, the SPEED at which treatment is initiated is ESSENTIAL in determining how the laminitic episode progresses, which is in two possible ways; subacute or chronic. Horses which progress to the subacute type of laminitis do not develop any radiographic changes. This is not the case in horses which develop the chronic type, as the connective tissue and hemidesmosomes holding the two lamellar layers starts to fail, resulting in a loss of attachment between the hoof wall and coffin bone.
What changes can we see on the hoof and in radiographs in cases of chronic laminitis?
Visual signs of chronic laminitis include:
- The sole of the foot is no longer concave (there should be a slight depression in the sole of the foot, however this is usually no longer present when a horse has chronic laminitis).
- A widening of the white line – the white line is the junction between the hoof wall and the sole, playing a role in protecting the foot. When it widens, it becomes easier for bacteria and foreign material to track up the hoof wall, resulting in disease and brittleness of the hoof.
- Formation of growth rings which are not parallel – the hoof grows from the coronary band and are usually 7-10 mm wide. In cases of chronic laminitis, the rings tend to be less uniform, becoming wider at the heels.

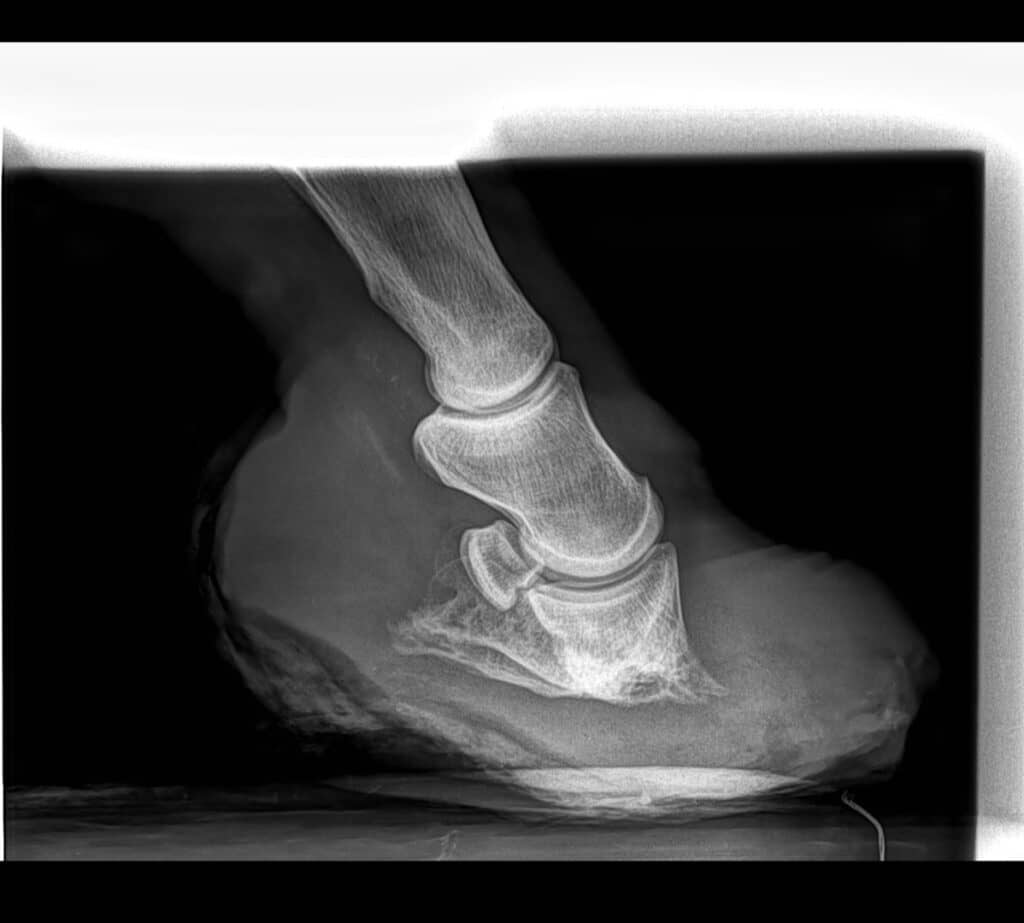
Radiographs are an essential tool in determining the severity and prognosis of the laminitis.
- Changes can include: Separation of the lamellae layers as the connection between the dermal and epidermal layers breaks down.
- Thinning of the sole due to compression from the coffin bone.
- Distortion of the area around the coronary band (you may see this visually as the hair may no longer point downwards).
- Eventually, remodelling of the coffin bone as more weight is carried through the toe of the bone, as opposed to through the sole.
If the laminitis is not treated accordingly, the horse will not become sound, having occasional flare-ups as laminitic episodes continue to occur. The widening of the white line, and subsequent bone disease can lead to the formation of more foot abscesses as the number of pathogens (bacteria) within the white line increases in chronically laminitic horses⁴.
As the sole depth decreases further (it should be 1.2-1.5 cm), the coffin bone is less protected from trauma, resulting in laminitic horses being more sensitive or foot-sore on hard ground. As this happens, the sole development slows down, resulting in a soft sole, causing further discomfort. As the white line breaks down and wider growth rings are produced at the heel, the foot eventually takes the shape of a slipper, as the hoof capsule grows forwards and upwards.
Eventually, if the collapse of the coffin bone is significant enough, the coffin bone may protrude through the sole, resulting in irreversible changes and a significant amount of pain.
If my horse gets laminitis, will I have to put him/ her to sleep?
Working as a vet, when warning owners about the risks of laminitis, and the importance of prevention and prophylactic care, this was a common question that I was asked. A 2020 study by Pollard et al.⁵ looked into the factors associated with euthanasia in horses and ponies that had laminitis. In the study, laminitic horses were more likely to be euthanised due to:
- Recurrent medical problems (such as colic)
- Remaining lame (or having a longer recovery time) after their most recent bout of laminitis
- Other lameness issues
- Poor hoof health
- Cushing’s disease
They were less likely to be euthanised if owners tracked their horse’s weight regularly, therefore recognising early changes in body condition. In my personal opinion, based on countless discussions with owners, maintaining the horse’s quality of life is generally far more significant, than financial implications associated with treating chronic laminitis.
Prevention
If you know that your horse may be at risk, albeit due to increased age, increased weight, presence of Cushing’s or equine metabolic syndrome (or signs associated with these diseases) or your pasture becoming too rich, it is your responsibility to make changes before laminitis occurs, or to notice the early signs. This can include monitoring your horse’s digital pulse and hoof temperature; an increase in both can be indicative of an acute laminitic episode being right around the corner⁶.
It is sensible to discuss how to feel for a digital pulse, your horse’s body condition score and risk factors with your regular vet, while ensuring that you are prepared for the worst case scenario. Taking radiographs early in the course of a laminitic episode will help you track whether the current issue is subacute or chronic and, help guide you towards the best possible treatment options.
Conclusion
I hope that an understanding of the anatomy of the foot helps to increase the importance of both prevention and early intervention of laminitis. As the infamous saying goes, ‘No hoof, no horse’; a healthy hoof – coffin bone relationship is an essential cornerstone in maintaining your horse’s quality of life.
Images courtesy of Equine Lameness Prevention Organisation
References
- Wylie, C., Collins, S., Verheyen, K. and Newton, J., 2012. Risk factors for equine laminitis: A systematic review with quality appraisal of published evidence. The Veterinary Journal, 193(1), pp.58-66.
- McGowan, C., Cooper, D. and Ireland, J., 2016. No Evidence That Therapeutic Systemic Corticosteroid Administration is Associated With Laminitis in Adult Horses Without Underlying Endocrine or Severe Systemic Disease. Veterinary Evidence, 1(1).
- Rucker A, Orsini J. Laminitis. In: Orsini J, Divers T, ed. by. Equine Emergencies: Treatment and Procedures. 4th ed. St. Louis, MO: Elsevier Saunders; 2014. p. 697-712.
- Onishi, J., Park, J., Häggblom, M., Fennell, M. and Fugaro, M., 2012. Chronic laminitis is associated with potential bacterial pathogens in the laminae. Veterinary Microbiology, 158(3-4), pp.329-336.
- Pollard, D., Wylie, C., Newton, J. and Verheyen, K., 2020. Factors associated with euthanasia in horses and ponies enrolled in a laminitis cohort study in Great Britain. Preventive Veterinary Medicine, 174, p.104833.
- Brown, H., 2019. Can changes in hoof wall temperature and digital pulse pressure be used to predict laminitis onset?. Veterinary Evidence, 4(4).
