Diseases & Conditions
Liver disease in horses
Stuart Davies discusses the possible causes, diagnosis and treatment of disease in this vital organ
The liver is involved in numerous different bodily reactions vital for life. Disease of the liver is common and can be due to toxic, infectious, neoplastic and endocrine causes. The liver is an amazing organ and can repair mild damage. However, hepatic (liver) failure occurs when function is reduced by roughly 70% or more. This does occur less commonly, but unfortunately, when it does it carries a much poorer prognosis for recovery.
Liver disease can be diagnosed based upon clinical examination, history of presentation and biochemical testing i.e., blood analysis. Clinical signs of liver disease can be non-specific including dullness, inappetence, photosensitisation, jaundice and behavioural changes. However, liver disease can also often be subclinical and found as an incidental finding on routine blood testing. Therefore, when a case has been identified testing of herd mates should be conducted in case of a common inciting cause, and to treat these prior to irreversible damage.
The diagnosis
There are multiple enzymes that will appear within blood once the liver has been damaged. These include Alkaline Phosphatase (AP), Gamma- Glutamyl Transferase (GGT), Aspartate Aminotransferase (AST) & Glutamate Dehydrogenase (GLDH). However, these can be derived from other sources, so interpretation should be made considering the whole clinical picture. If there is a suggestion of liver damage, it is imperative to assess if any impairment of liver function is present. This may be identifiable by the clinical pathology changes below:
- A hyperglobulinaemia (increased globulins) is identified after the immune barrier of the liver, called Kuppfer cells, are impaired and exposure to various antigens results in chronic stimulation of the immune system.
- Bile acids and bilirubin is usually elevated as the liver is unable to excrete the compounds from hepatocytes (the cells constituting the liver) or bile duct flow is obstructed.
- Low levels of albumin, hypoalbuminaemia, can be apparent following reduced production by the diseased liver.
- The liver is essential for the conversion of a cell waste product, ammonia, into urea, to enable excretion. Therefore, elevated levels of ammonia (hyperammonaemia) and reduced levels of urea can occur.
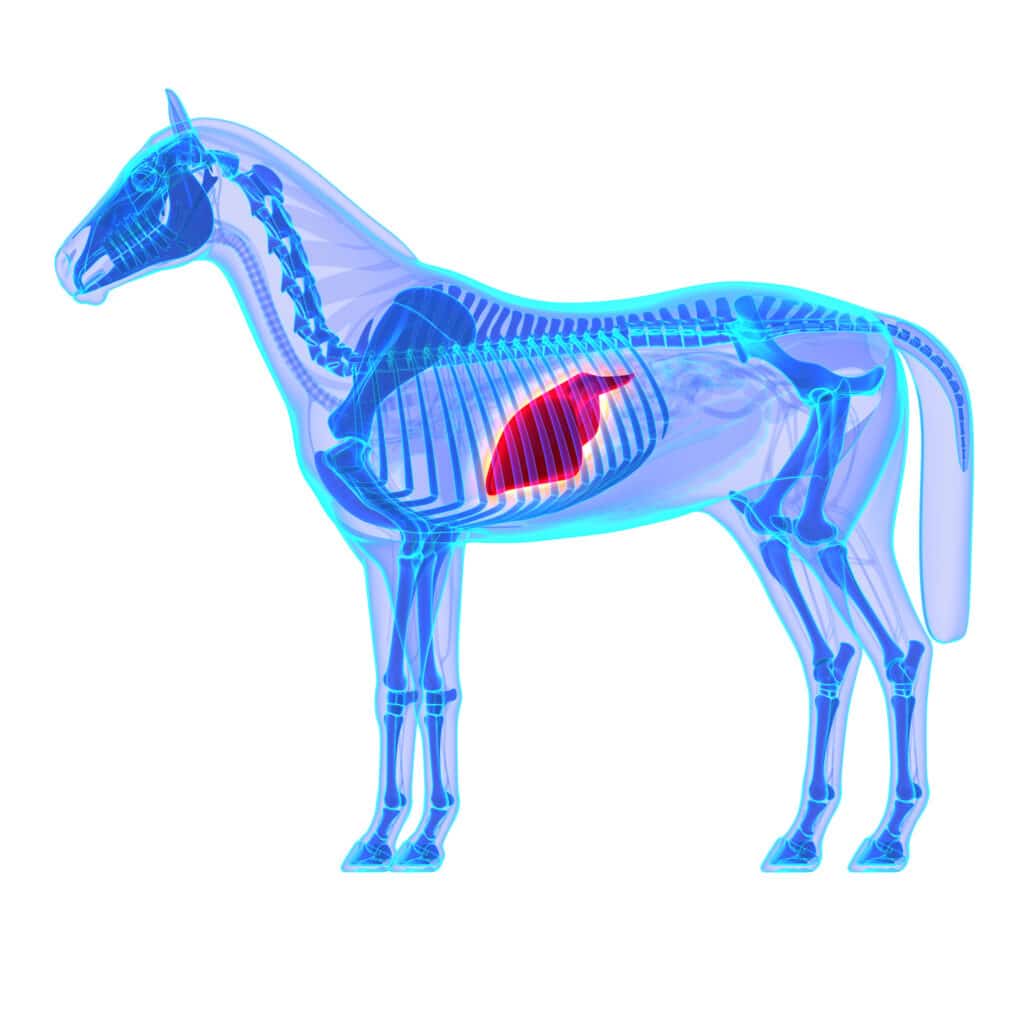
Bloods and clinical signs are suggestive of liver disease so what might be the next step? Ultrasonography of the liver can reveal whether there is a change in shape, margins, parenchyma (tissue of the liver) and diameter of bile ducts. Biopsy of the liver can be performed using ultrasound or additional blindly using bodily landmarks. The site is located at the 13th intercostal space (space between ribs) on a point between the point of the elbow and tuber coxae (point of the hip) on the right side.
Despite the liver being integral in platelet production and effective coagulation (blood clotting), excessive blood loss is not commonly reported. Assessment of biopsy samples allows confirmation of liver disease, identification of a cause, correct treatment, and an idea of prognosis.
“Ingestion of ragwort (Senecio jacobaea) is commonly implicated as a cause of liver disease”
Firstly, lets consider normal anatomy. The hepatocytes (cells of the liver) are arranged in regions called lobules, surrounded by a thin layer of connective tissue. At the corner of each lobule is a portal area. The portal area contains a hepatic artery, bringing blood in, a hepatic vein, taking blood away, bile ducts and lymphatic vessels, carrying cell waste products in tissue fluid. Blood and waste products are brought into the lobule whereby they are transferred to hepatocytes for them to perform their metabolism, detoxification function and then exit the liver via the hepatic vein, bile ducts and lymphatic vessels.
When a disease process occurs this initiates the inflammatory cascade; Inflammatory cells are drawn into the liver by chemical signals and these can be identified within hepatocytes and in portal areas. As cells are damaged, they become swollen and eventually die, appearing as small and condensed cells. Following damage areas of bleeding are visible as haemosiderin deposits. This is a deposition of iron, contained within haemoglobin, which is the oxygen carrying compound of red blood cells.

An increase in bile acid concentration and impaired bile excretion, can lead to visible stones within the biliary ducts, known as cholelithiasis. As mentioned above the cells of the liver can replicate to repair damage. However, when this happens repeatedly, and disease is classed as chronic, connective tissue is also deposited between divided cells. This scarring/ fibrosis appearance is classed as cirrhosis.
The connective tissue impedes the normal blood flow within the liver so high blood pressure, portal hypertension, occurs. Blood is ineffectively delivered to the liver resulting in metabolites not being detoxified. Higher vessel pressure leads to the leakage of fluid from vessels into cavities or, dependant parts of the body. Overweight animals with excessive fat deposits can mobilise these reserves when food is then restricted. This can lead to the adipocyte (fat cell) accumulation within liver cells.
Ingestion of Ragwort (Senecio jacobaea) is commonly implicated as a cause of liver disease, whether this be in dried form in forage or fresh in grazing. Usually, the disease presents itself sometime after the ingestion of the plant occurred. Pyrrolizidine alkaloids, the toxic compound within ragwort, leads to impaired hepatocyte replication. Despite cell replication being prevented DNA replication continues. This causes the formation of liver cells with an enlarged nucleus (DNA containing centre of cell) called a megalocyte.
- Nutritional management is vital in cases of hepatic lipidosis. Diets should be low in protein, to reduce ammonia production.
- Supplement Vitamin E & Selenium these can act as anti-oxidants and reduce the risk of Iron toxicity. These are usually in insufficient quantities in horse diets. Therefore, in hepatic disease cases when iron deposits are known to occur supplementation of these is presumed advantageous to prevent iron toxicity.
- Fluid therapy is beneficial to correct electrolyte disturbances, to enhance perfusion and to remove toxins.
- Corticosteroids may be necessary to reduce inflammation and formation of fibrosis.
- Antibiotics may be necessary if an infection is indicated.
- Lactulose can be given to remove ammonia from the blood and transport it into the intestine, to be excreted.
References
Bergero, D. and Nery, J. (2008), Hepatic diseases in horses. Journal of Animal Physiology and Animal Nutrition, 92: 345-355. https://doi-org.liverpool.idm.oclc.org/10.1111/j.1439-0396.2007.00798.x
DeNotta, S. L. and Divers, T. J. (2020) ‘Clinical Pathology in the Adult Sick Horse: The Gastrointestinal System and Liver’, Veterinary Clinics of North America: Equine Practice, 36(1), pp. 105–120. doi: 10.1016/j.cveq.2019.11.004
Dunkel, B., Jones, S., Pinilla, M. and Foote, A. (2015), Serum Bile Acid Concentrations, Histopathological Features, and Short-, and Long-term Survival in Horses with Hepatic Disease. J Vet Intern Med, 29: 644-650. https://doi-org.liverpool.idm.oclc.org/10.1111/jvim.12551
Gupta, R. C. (2018) Veterinary toxicology : basic and clinical principles. Third edition. Academic Press, an imprint of Elsevier
Young, Barbara, et al. Wheater’s Functional Histology, Elsevier, 2006. ProQuest Ebook Central, https://ebookcentral.proquest.com/lib/liverpool/detail.action?docID=1429548

